Abstract
Background: Understanding disparities in allograft access is a prerequisite to interpret outcomes. Moreover, while alternative donors extend access, the extent to which there are racial disparities in availability of optimal donors is not established.
Methods: We evaluated access to alternative donor allografts (all other than HLA-identical sibling donors) in adults 19-65 years according to recipient ancestry over time between 1/2016-4/2021. During this period an 8/8 HLA allele-matched unrelated donor (URD) had priority followed by double unit cord blood (dCB) (usually preferred if < 60 years) or haploidentical donors with mismatched URDs being considered most recently. We examined access to any acceptable donor, as well as an optimal donor, by recipient ancestry. To determine trends over time, we compared early (1/2016-1/2018, 25 months), middle (2/2018-2/2020, 25 months), & pandemic (3/2020-4/2021, 14 months) time periods.
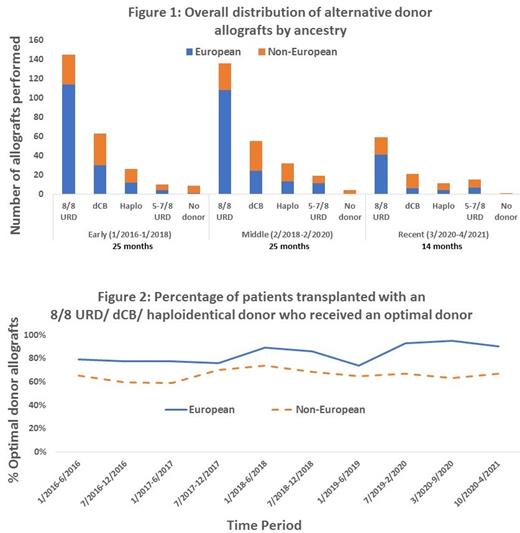
Results: 592 adults (median 53.5 years, range 19-65) received alternative donor allografts. 374 (63%) had European & 218 (37%) non-European origins (66 African, 56 Asian, 55 White Hispanic, 41 other). Overall, 340 (56%) patients received 8/8 URD, 139 (23%) dCB, 69 (11%) haploidentical, & 44 (7%) 5-7/8 URD grafts with 14 (2%) patients having no graft. Europeans (263/374, 70%) mostly received 8/8 URD donors, whereas only one-third of non-Europeans (77/218, 35%) did (p < 0.01). Moreover, non-European patients were more likely than Europeans to receive HLA-disparate donors of all types: 36% of non-Europeans received dCB vs 16% of Europeans, 18% vs 8% for haploidentical donors, 10% vs 6% for 5-7/8 URD grafts. African ancestry patients (n = 66) were the least likely to receive 8/8 URDs (13/66, 20%) with 27/66 (41%) of them receiving dCB, 16/66 (24%) haploidentical, & 10/66 (15%) 5-7/8 URD grafts. When analyzing by period, the relative proportion of patients receiving allografts from 8/8 URDs, dCB, & haploidentical donors remained unchanged over time (Figure 1). However, while 14 patients (13 non-Europeans including 11 of African ancestry) had no graft, the utilization of 5-7/8 URDs (4% of alternative donor allografts 1/2016-1/2018, 8% 2/2018-2/2020, 14% 3/2020-4/2021) has decreased the "no graft" incidence to 1% of patients most recently (Figure 1).
We then analyzed access to an "optimal donor" defined as an 8/8 URD < 35 years (Shaw et al., BBMT 2018), a dCB graft with each unit with a CD34+ dose > 1.5 x10^5/kg & > 4/8 HLA-match (Politikos et al., BBMT 2020), or a haploidentical donor < 40 years without recipient high titer donor-specific antibodies (McCurdy et al., Seminars in Hematology 2016 & others). Mismatched URDs were excluded based on lack of literature guiding an "optimal" definition. Of 8/8 URDs/ dCB/ haploidentical transplant recipients, 424/548 (77%) received an optimal donor with 269/340 (79%) URD, 94/139 (68%) dCB, & 61/69 (88%) haploidentical grafts being optimal. Transplanted non-Europeans were less likely to receive an optimal 8/8 URD / dCB / haploidentical donor than transplanted Europeans (67% vs 84%, p < 0.01) with White Hispanic & African patients having the lowest chances at 56% & 61%, respectively. Analysis of the 3 periods showed the likelihood that non-European patients received an optimal 8/8 URD / dCB / haploidentical donor is not improving: optimal allografts in 63% of non-Europeans vs 78% of Europeans 1/2016-1/2018, 68% vs 88% 2/2018-2/2020 & 68% vs 92% 3/2020-4/2021. Notably, the greatest disparity was seen at the pandemic's onset (3/2020-9/2020, Figure 2).
Conclusion: Our data suggests access to 8/8 URDs for non-Europeans is not improving but utilization of all potential alternatives (dCB, haploidentical, 5-7/8 URD) is increasingly providing "donors for all". However, when incorporating the concept of an "optimal" 8/8 URD/ dCB/ haploidentical donor, there is a significant disparity in access to optimal donors for non-Europeans, with Africans & White Hispanics the least likely to receive an optimal graft. This disparity is also not improving, and worsened at the pandemic's onset. Optimization of dCB, haploidentical, & mismatched URD transplants, & recognition of optimal donor definitions for each, is critical to further improve allograft outcomes. Future studies must also investigate the extent to which futile 8/8 URD pursuits adversely impact non-European patient transplant outcomes.
Politikos: Merck: Research Funding; ExcellThera, Inc: Other: Member of DSMB - Uncompensated. Giralt: AMGEN: Membership on an entity's Board of Directors or advisory committees; PFIZER: Membership on an entity's Board of Directors or advisory committees; JENSENN: Membership on an entity's Board of Directors or advisory committees; GSK: Membership on an entity's Board of Directors or advisory committees; CELGENE: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; SANOFI: Membership on an entity's Board of Directors or advisory committees; JAZZ: Membership on an entity's Board of Directors or advisory committees; Actinnum: Membership on an entity's Board of Directors or advisory committees. Gyurkocza: Actinium Pharmaceutical Inc.: Research Funding. Perales: Omeros: Honoraria; Novartis: Honoraria, Other; NexImmune: Honoraria; Nektar Therapeutics: Honoraria, Other; MorphoSys: Honoraria; Miltenyi Biotec: Honoraria, Other; Merck: Honoraria; Medigene: Honoraria; Kite/Gilead: Honoraria, Other; Karyopharm: Honoraria; Incyte: Honoraria, Other; Equilium: Honoraria; Cidara: Honoraria; Celgene: Honoraria; Bristol-Myers Squibb: Honoraria; Sellas Life Sciences: Honoraria; Servier: Honoraria; Takeda: Honoraria. Ponce: Ceramedix: Consultancy, Honoraria; Takeda Pharmaceuticals: Research Funding; CareDx: Consultancy, Honoraria; Kadmon pharmaceuticals: Consultancy, Honoraria; Seres Therapeutics: Consultancy, Research Funding; Generon Pharmaceuticals: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal